WWJD - What Would Joseph(ina) Do, Case 1.
You are Joseph(ina).
You are a Corpsman/medic doing sick call at the local Base hospital. You pissed off someone, so you are stuck with the overnight shift.
A 46 y.o. male comes in with CP x 1 hour. He had an MI 7 years ago requiring 2 stents.
His EKG looks funny but not diagnostic. By this I mean, it looks like it showed a previous inferior MI but you don't have an old one to compare it to.
As you are talking to him, his eyes roll back, he becomes unresponsive.
You establish that he is unresponsive, you check pulses (not there) and you look at the rhythm strip:
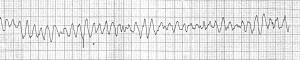
(copied from Medblog)
What would YOU do?
Hint #1:
Step 1: _______
Step 2:_______
Step 2a:______
Step 2b:______
Step 3:_______
Hint #2: There are only 3 things you really need to do to revive this dead man. Yes, he is dead. You have a very limited time to undead him.
Hint #3: KISS rule. Permissive hypothermia, surgery, anti-arrhthmics, ECMO, etc will not save this guy right now.
You are Joseph(ina).
You are a Corpsman/medic doing sick call at the local Base hospital. You pissed off someone, so you are stuck with the overnight shift.
A 46 y.o. male comes in with CP x 1 hour. He had an MI 7 years ago requiring 2 stents.
His EKG looks funny but not diagnostic. By this I mean, it looks like it showed a previous inferior MI but you don't have an old one to compare it to.
As you are talking to him, his eyes roll back, he becomes unresponsive.
You establish that he is unresponsive, you check pulses (not there) and you look at the rhythm strip:
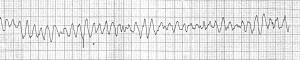
(copied from Medblog)
What would YOU do?
Hint #1:
Step 1: _______
Step 2:_______
Step 2a:______
Step 2b:______
Step 3:_______
Hint #2: There are only 3 things you really need to do to revive this dead man. Yes, he is dead. You have a very limited time to undead him.
Hint #3: KISS rule. Permissive hypothermia, surgery, anti-arrhthmics, ECMO, etc will not save this guy right now.
Last edited:
